Inborn errors of immunity (IEIs) are a heterogeneous group of monogenic diseases that cause impaired development or function of the immune system. Historically, IEIs were considered diseases that lead to susceptibility to severe infections. David Vetter (aka the bubble boy), the most mediatic case of these diseases, was born with an IEI that causes the absence of T and NK cells and, consequently, susceptibility to multiple severe infections. Interestingly, in the past few years, the clinical spectrum of patients with IEIs has expanded to encompass other clinical manifestations such as autoimmunity, allergy, autoinflammation, or cancer. Nowadays, there are about 500 known genetic causes of IEIs, and their study is instrumental in providing a genetic diagnosis for patients, counseling for families, and applying preventive treatments for individuals at risk. Furthermore, these patients, often “knockouts” of specific molecules, provide a unique opportunity to understand the mechanisms of human immunity without relying on artificial models. However, despite all the advances in the field, about half of the patients with a suspected IEI of immunity lack a genetic diagnosis, and in a sizeable fraction of patients with genetically diagnosed IEIs, the pathological molecular mechanisms of the mutations remain elusive. Furthermore, despite compelling evidence that a single gene mutation can cause severe infections by a specific pathogen, most infectious diseases have not been studied as IEIs. Through an international network of collaborators, our lab recruits and studies patients with IEIs of unknown genetic etiology, patients with genetically defined IEIs of unknown molecular mechanism, and patients with selective susceptibility to specific infectious agents. Using next-generation sequencing, we identify new genetic causes of IEIs. Furthermore, employing a multidisciplinary approach combining molecular biology, biochemistry, human immunology, computational biology, and multi-omics, we functionally characterize the mutations responsible for the diseases in our patients. Finally, our lab leverages the basic molecular, immunological and biological insights from studying these patients to develop new immunomodulatory approaches for common diseases like cancer.

IEIs are grouped in different categories according to the arm of the immune system they affect and their clinical presentation. These groups are; defects of T cell development or function (combined immunodeficiencies), antibody deficiencies, diseases of immune dysregulation, congenital defects of phagocytes, defects in intrinsic and innate immunity, autoinflammatory diseases, complement deficiencies, bone marrow failure, and phenocopies of IEIs. The clinical presentation of IEIs is variable and includes severe or unusual infections, autoimmunity, autoinflammation, severe allergies, and malignancies. Although each type of IEI is considered a rare disease, in aggregate, their prevalence is approximately 1 in 1,000 to 5 in 5,000 individuals. Despite the improvement in understanding the genetic and molecular causes of IEIs that have occurred during the past decades, a large percentage of patients with IEIs lack a genetic diagnosis, or the molecular mechanism that causes the disease remains unknown. Through an international network of collaborators, we recruit families with suspected IEIs. We then use a combination of next generations sequencing, human genetics, immunology, biochemistry, molecular biology, multi-omics, and computational biology to discover and characterize IEIs. Read more.

In addition to IEIs that cause immune deficiencies, many IEIs result in enhanced inflammatory responses that can be harmful and culminate in deadly autoinflammatory or autoimmune diseases. The in-depth functional characterization of mutations causing this type of IEIs provides valuable information on how to drive the human immune system toward activation and inflammation. Hence, these diseases provide a platform to directly translate insights from human genetics to efforts to engineer immunity and increase the efficacy of immunotherapy. As proof of concept, deficiencies in the two most widely used immune checkpoint inhibitor antibody targets, CTLA4 and PD-1, are also the genetic causes of monogenic IEIs with severe autoimmunity. Yet, the knowledge obtained from studying IEIs causing autoimmunity and autoinflammation has not been broadly leveraged for therapeutic purposes. We hypothesize that IEIs provide natural experiments and human genetic insight to direct new approaches to immune system engineering for immunotherapy. Hence, we exploit the knowledge from studying IEI to manipulate innate immunity activation for immunomodulatory purposes.
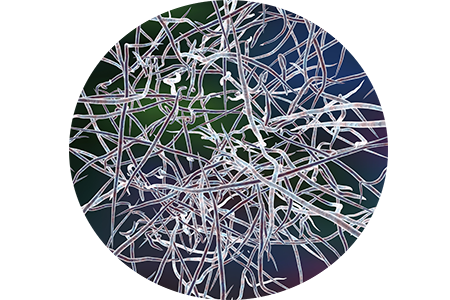
Nocardiosis is a severe infectious disease caused by the gram-positive bacteria Nocardia spp. Although it is commonly accepted that exposure to it is universal, only a small fraction of exposed individuals develop the disease, with the vast majority remaining asymptomatic or healthy. Nocardiosis has been described as a disease of immunocompromised patients suggesting that exposure to the pathogen is necessary, but a host predisposition is also required. Interestingly, increasing numbers of cases of nocardiosis in individuals without any other identified risk factors are being reported monthly. Under the hypothesis that nocardiosis in otherwise healthy individuals is an undiagnosed IEI, we are recruiting a growing cohort of patients with this disease and performing genetic and immunological studies. Read more.
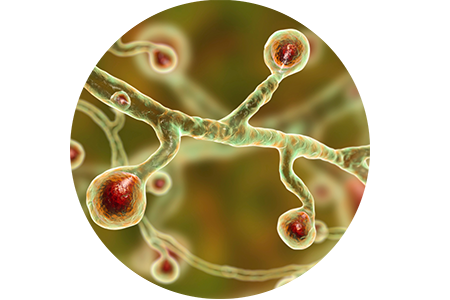
During recent years the global burden of fungal diseases has been steadily increasing. Among them, the endemic mycoses are a diverse group; each occupies a specific ecologic niche in the environment. In the US, three fungi species are considered endemic: Histoplasma capsulatum, Coccidioides spp. , and Blastomyces dermatiditis causative agents of histoplasmosis, coccidioidomycosis, and blastomycosis, respectively. These fungi usually grow in soil, decaying vegetation, and exposure occurs when individuals inhale their conidia or spores. In the lungs, the conidia or spores develop into a yeast or spherule phases, capable of causing pulmonary disease. In most cases, individuals remain asymptomatic, subclinical, or have a self-resolving flu-like episode that goes undiagnosed. However, in other cases, the disease can progress to acute respiratory distress syndrome (ARDS) or disseminate to potentially any organ in the body. When dissemination occurs, morbidity and mortality dramatically increase. The observation that patients with acquired immunodeficiency caused by HIV or immunosuppressive medications are more prone to develop severe disease suggests that these diseases in otherwise healthy individuals may be due to inherited immunodeficiency. We are tackling this hypothesis by genetically studying these patients in search of new IEI causing susceptibility to these pathogens. Read more.